Walking around Robert Wood Johnson University Hospital’s (RWJUH) Buildings, I saw a sign that said, “Heroes Work Here.” This sentiment is common and echoed by the public, businesses, and hospitals alike. However, I quickly realized that heroes are expected to work understaffed and to the point of exhaustion.

Being a hero is not just about hard work and dedication— it is about doing your job under challenging and stressful conditions.
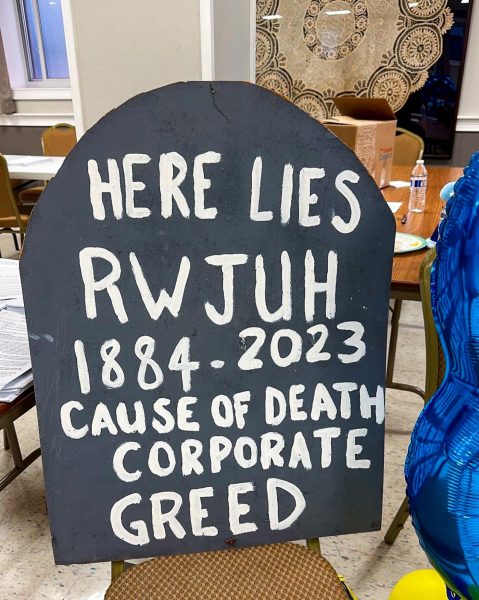
As I left the car and started walking around the streets surrounding Robert Wood Johnson University Hospital, I noticed a huge inflatable rat holding a sign reading “NURSES ON STRIKES: SAFE STAFFING SAVES LIVES.” It was a clear message to RWJUH: These nurses would not give up until they had the necessary regulations they were protesting for. The rat was placed next to a church building across the street from Robert Wood Johnson University Hospital. A sprawl of people outside were still holding the picket line. There were dozens more nurses inside the church basement where most of the interviews featured in this article were held.

Moreover, I realized something striking as I sat and listened to nurse after nurse describe their experiences: the people in that room and on that picket line had known each other for years– decades even. There was a sense of community amongst them. Despite the long months of picketing and differing opinions, the nurses here could sit and talk to each other with endearment. People were drinking coffee and eating cheesecake, laughing and joking as they discussed a decision that would impact their careers. They were all waiting for the meeting to start.
Midway through the assembly, a man started speaking and then— “Can you speak louder!” A voice from the back asks. The man smiles and makes his voice comically loud— “Is this loud enough for you, m’lady?”. It is a small example of the laughter and joy held by these nurses. I can see why Judy Danella is the president of the union. She is confident, strong, and witty. The nurses at RWJUH are some of the strongest and smartest people I have met. Furthermore, their experiences deserve to be heard, understood and shared with the thousands of current and future nurses.
WHO AND WHAT IS RWJUH?
To understand the strike itself, you first need to understand the system. Robert Wood Johnson Barnabas Healthcare (RWJ Barnabas) system is the “largest integrated health care delivery system” in New Jersey. They are an organization of hospitals, schools, and clinics throughout the state. The striking nurses in this article were specifically a part of the Robert Wood Johnson University Hospital in New Brunswick, New Jersey.
So, what is a strike?
A strike occurs when a group of people under a specific company or industry decide to withhold their labor to improve their working conditions. That group of people can be in a union, but it is not necessary to be a part of a union to strike. A labor union is a group of employees in a specific trade, industry, or corporation organized to protect employees and stop exploitation collectively. In this case, the nurses striking were under a United Steelworkers Union (representing workers in metallurgical, healthcare, and other service industries) contract— USW Local 4-200.
Unions and employers must draw up a contract to set the workplace standards. These contracts typically expire every 3-4 years. The previous contract between RWJUH and the USW Local 4-200 lasted from July 1, 2020 to June 30, 2023. During a contract’s duration, union workers cannot strike. They can only strike before a contract takes effect or after it expires. When a contract has expired, negotiations are held between employers and the union to set new contract terms. If both sides cannot reach an agreement, the union will hold a vote, and members will decide if a union should go on strike. In this case, there were months of negotiations between USW 4-200 and RWJUH. These negotiations started on April 10, 2023. The hospital and union leaders created a Memorandum of Agreement (MOA), a written document between two parties that describes how both parties will work together to meet a common objective. However, when the MOA document was shown to the nurses union, members rejected the document. There were more negotiation meetings, but the hospital and union could not agree on varying issues, especially the nurse-to-patient staffing ratios. The unionized nurses wanted safe staffing conditions, which RWJUH refused to provide. Due to this, nurses began striking on August 4, 2023.
There are two types of strikes— unfair labor practice strikes (ULP) and economic strikes. ULP strikes occur when employers violate federal labor laws. RWJUH had not violated any federal labor laws at the time of the strike. This means the nurses were utilizing an economic strike, which is held to pressure employers to meet certain standards.
The Unfair Treatment of Nurses
Nurses across America are treated poorly. This article primarily focuses on the mistreatment of nurses who worked in Robert Wood Johnson Barnabas, but every experience written down is just one out of thousands.
How are Nurses Treated Poorly?
Nurses in America are overworked to the point of burnout. A study by the American Nurses Foundation (ANF) reported that 56% of surveyed nurses experience symptoms of burnout.
Nathalie Canton McDonald, a nurse at RWJ, said, “It was quite exhausting. Just– going in every day”.
Faith, a float pool nurse, said that “walking in, [she] had a wave of anxiety” over “not knowing what [her] shift will be like.”
Constant exhaustion and anxiety are symptoms of burnout, which is a chronic issue in the healthcare system. Burnout in nursing comes from many issues inherent to the job (long hours, providing emotional care to others, etc.) and their personal lives, but also due to systemic failure on the part of the American healthcare System. The biggest reasons for burnout include insufficient wages, too many tasks, poor leadership, and inadequate staffing. These issues can lead to emotional exhaustion, frustration, negative feelings about one’s job, apathy, etc.
However, burnout is just a symptom of systemic failure– so what are the causes?
Nicole said, “There are [too] many times I have to go to the bathroom, but I don’t—I hold it in because my patient needs something. Or I would not have lunch until 3 or 4 p.m., and I started my shift at 7:00 a.m.”
A lack of bathroom breaks and poor nutrition can lead to further exhaustion and even poorer health for nurses.
Many nurses also would not go home on time. One reason is the number of tasks they must complete, including patient care, inventory, and charting. But the biggest problem is the patient-to-staff ratios.
“We don’t have a ratio,” mentioned Julia.
Ratios refer to the number of patients that one nurse handles. However, because there were no mandated ratios, the number of patients a nurse handled at RWJUH became overwhelming.
“We could have 1 or 2 nurses working out there and could wind up having 6-7 patients at the worst,” said Julia. Nurses spend a good portion of their shifts helping patients’ bodies recuperate. They all require individualized care due to different ages, situations, injuries, illnesses, treatments, equipment, etc.
But this means their administrative tasks are pushed aside until they find the time. However, that “time” is often after their shift should be over. Nurses also can’t leave those tasks to others (partly because there are no “others” considering the short staffing issue)– which means they cannot leave until they finish those tasks.
“My shift is supposed to start at seven a.m., and it’s supposed to end at 7:30. But most days, I would not leave until 8:30…that was a daily occurrence,” said Nicole.
Overtime was a constant presence for these nurses. While New Jersey is not among them, there are about 32 states that require mandatory overtime for nurses. These laws ensure that the safe staffing levels in the legislature are met. However, due to the current nursing shortages (both in RWJUH and hospitals across the country), many healthcare facilities need nurses to work overtime to get by on a work shift without serious issues (and meet state legislature in the case of the 32 states mentioned). It’s a short-term solution to a long-lasting issue.
However, organizations like the American Nurses Association believe that “mandatory overtime is an unacceptable solution to appropriate staffing levels.” This is likely because overtime (of any kind) can lead to burnout and fatigue, which is unsafe for a nurse’s ability to do their job and a patient’s care.
In another instance of working overtime, “[RWJ workers] schedule procedures the day before. And unfortunately, going into most days, they already know we’re going to be short staffed… more procedures than are physically possible to happen in our operating hours are put on the schedule… [which] forces people to have to volunteer to stay late because they know that they’re booking more procedures than we are physically capable of making happen in a regular day with our normal short staffed [nurses]” said Alice, a nurse in the cardiac-catheter lab.
This issue is exacerbated by the loss of many nurses in the lab—around 15—whose positions were never filled. This highlights another issue—specific problems arise in each department as a result of poor staffing. These issues are left unmanaged. However, many of those issues lead to the same effects—feeling fatigued, overwhelmed, and unsupported.
“At the end of a shift, there are many times where when I get home, and I see the lights on in my house, I will drive around the block so that I don’t have to talk to anybody. Until I see the lights go out, I know everybody else is in bed, then I go home,” said Alice.
They couldn’t just hang up their jobs when they left those hospital doors—it affected them when they left, and it affected their families, too.
They didn’t get enough time with their families to relax and rest. The work-life balance for these nurses was tipped in favor of work—at their expense.
Out of every experience and story I listened to throughout these interviews, this sentence impacted me the most. Family members play a crucial part in helping a person with their struggles by providing emotional and physical support. Additionally, spending time with family can improve people’s stress levels and overall mental health. By feeling constantly stressed at work and unable to spend time with their families, these nurses’ mental health was left under-prioritized and ignored.
Riley, another nurse at RWJ, said that he felt “Just overworked and just not feeling great about not being able to give 100% of [himself] to [his] patients because there’s just not enough of [the nurses] to go around for the patients”.
Poor staffing ratios do not affect nurses and lead to patients receiving care that could have been much better. But four experiences stuck out to me in all the interviews.
“One patient makes such a big difference because, say, someone’s looking for pain medicine, someone’s looking for that, then they’ll have to wait a little bit longer because that one extra patient can sometimes… require a little more of your time,” said Nicole.
“I’ll have patients that need to go off the unit for procedures and… I have to go with them because… they can’t go by themselves, so I’ll have to leave my other 3-4 other patients with another nurse with her set of patients, and I know that the nurse isn’t really paying attention to my patients,” said Faith.
“But I had other patients– they’re told they’re having surgery; they’re not prepared mentally for that. They’re lying in the bed crying. But I’ve got to leave them… They’re there, and you hear them crying. And you want to go to them, but you can’t. Because you’re in with the next patient… If you had enough nurses out there, you would have that time to give that personal touch. And sometimes that’s bigger than anything I can do for them physically,” said Alice.
It speaks to how many tasks a nurse needs to accomplish—healing a patient’s body, being emotionally present for patients, and finishing administrative tasks are some of the biggest duties they must complete. However, poor staffing ratios can lead to those tasks being done unsatisfactorily or put to the side for later, which is a difficult situation for patients and nurses alike.
“I actually was a patient here. I had cancer. I had 2 different types of cancer in 2015. And through 2017, I was a patient. Many many times. And my nurse friends (gestures to her colleagues) would come in on their breaks, if they got one, or they would come at the end of their shift just to make sure that I had gotten my medicines. That I had gotten bathed that day. That my sheets were changed on my bed that day, because I was post-surgery. I had one of my coworkers– he slept at my bedside okay [for 5 days in a row]? But it shouldn’t be that way,” said Alice.
How scared can a coworker be of you not receiving the care you need due to poor staffing ratios, to the point that they sleep next to you for days?
What if you do not have someone to help you and be here for you like that?
All these nurses wanted to provide their patients the best care they could provide— but poor staffing ratios were holding them back. Not every nursing experience can be shared here— but there were so many more. There are many more that are not written.
Thousands.
It is a chronic issue.
However, it never needed to be chronic. Many nurses had brought these issues forward a long time ago.
“Our main thing was that we kept asking for more help, and we just kept being told, ‘It was coming, it was coming.’ And it just didn’t come.” said Nicole.
This fact has been true for decades.
“I’ve been in the department for 35 years; I can’t remember it not being this way,” said Alice.
There is no work environment in which issues do not arise. However, RWJ was alerted to numerous issues by staff, which were previously ignored.
“Oh, they are acutely aware of [these issues], yes.”
There were even meetings held with management and upper administration to address the issue, but as Faith put it, “the same concerns were brought up again and again and it didn’t ever feel like there was ever any resolution to the concerns that were continuously brought up.”
RWJUH—and many hospitals like it—had problems that I believe should have been solved when first brought to someone’s attention. In my opinion, that is the worst aspect of this strike. This—120 days and millions spent on replacement nurses—did not need to happen. If there were safer staffing regulations and a better work environment, there would be no incentive to strike and every incentive to continue working.
However, the issues just continued rising, and the meetings over new contracts continued to be unsuccessful. So, the nurses at RWJUH knew what they needed to do—strike.
THE STRIKE
The nurses at RWJUH started striking on August 4 and continued for over 120 days. Throughout the strike, the hospital and the striking workers had numerous issues.
At the start of the strike, the nurses at RWJ were striking along with dozens of people on Little Albany Street. However, the hospital had filed an injunction against the striking nurses. This limited the number of people who could walk the picket line simultaneously. This was due to numerous incidents between striking nurses and security, noise disruptions, and obstructing working employees from leaving the hospital parking garages. The injunction was filed based on inconveniences. But its effect on the strike was much larger than an inconvenience.
“Nobody wanted to [be on the picket line] anymore after we got the injunctions,” said Alice.
After the injunction was filed, the only noise the picketers were allowed to make was their voices through banning megaphones, drums, etc. RWJUH made it much more difficult for nurses to strike against them. However, they could not stop the nurses from the act of striking itself.
Additionally, there were issues during the mediation.
The “RWJ team sat in one room, and the union team sat in another room. They didn’t even see each other. The mediator would run back and forth between the two rooms… And they would make them sit there for hours. 10-12 hours. Sometimes until 1 a.m.” said Alice.
However, while all of these things can be considered unfortunate, for me, the most horrific thing comes in the form of the nurses’ healthcare.
“They cut off our health insurance after a month of striking. We ha[d] no insurance,” said Nicole.
Numerous nurses at RWJ have their families on their hospital insurance plans. By cutting off the striking nurse’s health insurance, RWJUH did not just impact the striking nurses— they impacted their families, too. Healthcare is extremely expensive in America, of which a hospital would be fully aware. It is shockingly ironic. Cutting healthcare can also strain families due to the stress and worry that arise. After all, what if a family member falls sick? What if they have a chronic illness? What if they had ended up in an accident? Although there are subsidized health care packages (like Obama Care), households can run into the issue of one spouse making too much money to qualify for a good subsidy. This results in households making too much to qualify for enough money but making too little to afford proper healthcare for their entire family.
In my opinion, cutting the nurses’ healthcare was callous. This hospital provides some of the best healthcare for its patients. Yet, it made it more inaccessible for healthcare workers to receive care. It’s the most sardonic sentence I have heard. How can you be a healthcare provider yet make it more difficult for potential patients to receive care?
The Wider Issue
The problems at RWJUH were not limited to that hospital. The issues covered in this article are nationwide problems in healthcare, which have led to strikes nationwide. In 2023, there were 36 strikes in hospitals across the United States, an increase of 11 hospitals from 2021.
Some of the issues include but are not limited to inadequate staffing issues (28 hospitals), poor salaries (16 hospitals), nurse retention issues (7 hospitals), nurse retention issues (7 hospitals), unfair labor practices (7 hospitals), poor negotiation tactics and anti-union policies (6 hospitals), unsettled or unfair contracts (6 hospitals), and workplace violence (4 hospitals).
The striking nurses are not the only nurses enduring unfair working conditions. However, they are setting a standard for their hospitals (and hospitals around the country) to treat them with respect and dignity.
Because when hospitals do not treat nurses with respect and do not feel capable of fighting for better conditions, nurses start leaving the profession. There is a nationwide crisis of nurses leaving healthcare— especially since the COVID-19 pandemic in 2020. In 2021, around 100,000 nurses left their jobs. In a survey by AMN Healthcare, 94% of nurses say there is a moderate or severe nursing shortage in their area.
In RWJUH, Alice noticed how “newer nurses are coming out and coming into this hospital and realizing that they can get a better training opportunity and more experience and not have to work as short staffed and as critical… somewhere else.”
What have these poor conditions led to? How has this affected patient care?
THE STRIKE OUTCOME
By December 15, 2023, RWJUH and USW Local 4-200 had agreed on a contract. The hospital and nurses agreed that the nursing ratios were critical. The nurses went back to their jobs starting January 1, 2024. The contract will last for the next three years. The deal provides safer staffing ratios for patients and workers alike. However, it would not have been possible without this strike and without the workers who fought for and led it.
HOPE
No part of this article was easy to write. No part which I didn’t feel upset or angry or saddened by the poor staffing policies that our healthcare system has clung onto. But we can’t lose hope in our healthcare workers and larger system either.
There is one thing that we, as residents of New Jersey, potential healthcare workers, and students, can do. We can bring awareness to these issues, support bills and laws that would result in safe staffing ratios being instated on a state-wide level, and most importantly, listen to nurses and other healthcare professionals about their experiences.
This issue is a big one. However, it is not impossible to solve. Through community, laws, and effort, we can work towards fixing these problems for the future nurses at Piscataway High School.
Note: Although they did not request it, the names of the nurses interviewed in this story have been changed in order to protect their identities, due to the fact that the nurses’ strike recently concluded and tensions are still high on both sides.